Wesley Research Institute
Wesley Research Institute, formerly Wesley Medical Research, is focused on providing immediate improvements in patient care and quality of life through applied medical research.
The Task:
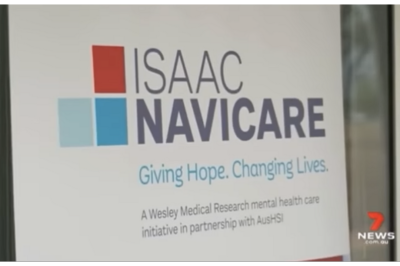
Wings Public Relations was appointed in November 2021 to support the launch of ISAAC Navicare in Moranbah, with the aim of enhancing access to mental health services and improve mental health outcomes in the Bowen Basin. This project involved strategy planning and tactical implementation including development of media alert and media release, liaison with media, on-site coordination, a video newsreel, short launch event video suitable for various stakeholder websites and still imagery. The successful outcome led to further appointments in 2022 including the promotion of the ministerial launch of a clinical trial to test treatment for the rare childhood genetic disorder Ataxia-telangiectasia (A-T) and the launch of a long-awaited clinical trial to help define a safe level of gluten exposure for all.
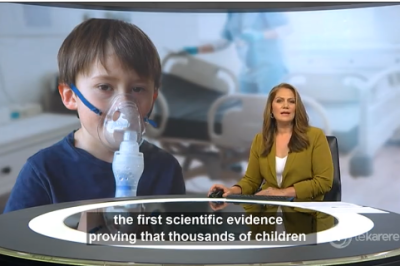
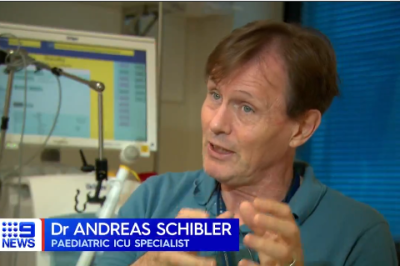
On 5 January 2023, the Wings Public Relations team was appointed to promote the world-first Australian and New Zealand study that delivered the first scientific evidence proving that thousands of children with respiratory disease can be safely treated in their local hospitals without the need to be transferred to a large hospital. With less than two weeks to develop a strategy and complete implementation, the Wings Public Relations team, working closely with the Wesley Research Institute, Chief Investigator Dr Andreas Schibler and his fellow researcher Dr Donna Franklin, managed to secure significant national and international media coverage reaching a cumulative potential reach of more than 1.3 million and an ASR of almost AUD $500,000. The breakthrough research from the Paediatric Acute Respiratory Intervention Studies (PARIS) II study was published on 18 January in the pre-eminent peer-reviewed Journal of the American Medical Association (JAMA).